|
A brisk walk a day keeps the doctor away by Fran Lowry Getting your patients tochange their unhealthy lifestyle habits can go a long way to improving their risk profile for cardio-vascular disease, experts say. Exercise and weight reduction work extremely well to lower cholesterol and blood pressure, especially in sedentary, obese individuals, says Dr. Steven Grover, professor of medicine, epidemiology and biostatistics, McGill University
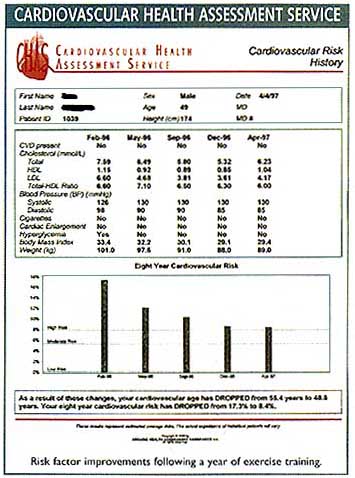
"The combination of exercise and weight reduction can have a huge impact. That's where the real synergy is. It not only lowers LDL cholesterol and raises HDL cholesterol, it lowers blood pressure and reduces glucose intolerance as well," Dr. Grover, who is also director of the cardiovascular health improvement program at McGill, and director of the division of clinical epidemiology at the Montreal General Hospital, told Cardiology Post in an interview. While exercise and weight loss won't work for everybody, they will allow many patients to at least decrease the amount of medication they are taking. And in a substantial proportion of patients, particularly those with moderate lipid abnormalities and mild hypertension, exercise and weight loss may be all that is needed to bring them under control, Dr. Grover said. He and his team of researchers have recently completed a study look ing at the cost-effectiveness of exercise to reduce cardiac risk through its impact on lipids and BP. That study is pending publication this spring. These lifestyle changes have the most benefit for people who are overweight and sedentary. "If you are already running marathons and you're thin, there isn't a whole lot more you can do to improve your situation. But take a sedentary, obese person, and there's a lot of room for improvement," Dr. Grover noted. Working out for approximately 30 to 40 minutes, 3 to 4 times a week, at 65% to 85% of maximal heart rate, should do the trick. Emerging guidelines from the Canadian Cardiovascular Society and Health Canada recognize the importance of exercise to reduce cardiac risk factors. With more than 60% of Canadians shunning exercise, there is a lot of room for improvement just by incorporating this lifestyle change. The majority of type II diabetics have the disease because they are overweight and sedentary. Getting off the couch and into running shoes would go a long way towards cardiac disease prevention. People really do respond," said Dr. Grover. Eight to 12 weeks will determine whether a patient will respond or not. Most sedentary, overweight people will respond. "I'd say well in excess of 80% will improve, based on our cardiac rehabilitation experience to date. We're talking a lot! The critical issue is, once they respond, and you prove to them that it works, to keep them going," Dr. Grover said. Unfortunately, by the end of a year it is not uncommon to find that anywhere from 30% to 50% of patients have given up their good habits and stopped exercising and watching their weight. Compliance, therefore, becomes a crucial factor in cardiovascular risk reduction, Dr. Grover noted. Giving patients feedback is key to getting good compliance. When patients start to back off from their exercise, or they gain a few pounds, it's time to show them that their lipids and BP are getting out of control. This means following your patients carefully. Before starting a patient on an exercise and weight reduction regimen, it's important to get baseline values of lipids and BP. Patients over the age of 45 who also have one or more risk factors for cardiovascular disease should also be given a stress test before they start in with vigorous exercise, to make sure they have no underlying cardiac disease. "The worst thing in the world you can do is to take a sedentary person, tell him to go out and start jogging, and then he goes and develops cardiac ischemia because nobody realized he had underlying atherosclerosis, so you have to be careful. Start them slowly and gradually. The biggest mistakes people make are that they either don't exercise at a sufficient intensity or they overkill in the first week or two and they hurt themselves and then they are finished," Dr. Grover warned. To make sure your patients are exercising at the right intensity, it's a good idea to send them to an exercise physiologist, where they can be supervised properly. Physicians should write a prescription for exercise for their sedentary patients, the same way they write prescriptions for drugs, suggests Ilka Lowensteyn, PhD, who works with Dr. Grover. She is an exercise physiologist and coordinator of the cardiovascular health improvement program - which is associated with the McGill University teaching hospitals. All major cities in Canada have cardiac rehabilitation programs, which should have a list of qualified physiotherapists and trainers who can guide the exercise program. ressure. Physicians can also check out the Canadian Association of Cardiac Rehabilitation's web site at www.cacr.ca for more information. There is always an increased risk of an event when you exercise, but if you don't exercise, the risk is even greater, says Dr. Lowensteyn. At the end of 12 to 16 weeks, reassess the situation. If there is a positive effect, urge patients to keep up the good work. But if there is no improvement, it's time to consider medication, Dr. Grover said. 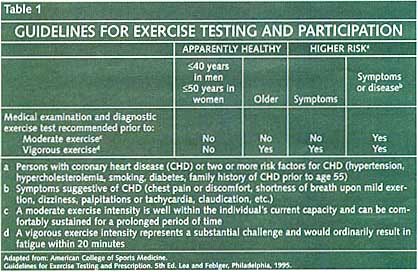
|